Leaders and Meetings
Who is a LLL Leader?
A La Leche League Leader is a mother who has had a specific type of breastfeeding and parenting experience, meets the prerequisites for Leadership, completed specific reading and introspection and has finished the extensive written training curriculum established by LLLI. A Leader upholds the Philosophy of La Leche League International.
Can I attend meetings as an expectant mother?
Yes, we encourage pregnant moms to attend a complete four meeting series in preparation for breastfeeding.
Can I bring my baby/children to the meeting?
Yes, children are welcome. We encourage nursing babies to join mothers at the meetings.
Can I bring my mother/mother-in-law/husband/other support person?
In general, we welcome support people to come. It is preferred that male support people do not attend the bulk of the meeting but instead come in at the very beginning of a meeting or at the very end.
Do you make home visits?
Some Leaders do make home visits, but it is not required of LLL Leaders. If you need help immediately, and the next LLL meeting in your area is not soon enough, contact a Leader in your area to see if there are any nearby Leaders who will meet with you.
A La Leche League Leader is a mother who has had a specific type of breastfeeding and parenting experience, meets the prerequisites for Leadership, completed specific reading and introspection and has finished the extensive written training curriculum established by LLLI. A Leader upholds the Philosophy of La Leche League International.
Can I attend meetings as an expectant mother?
Yes, we encourage pregnant moms to attend a complete four meeting series in preparation for breastfeeding.
Can I bring my baby/children to the meeting?
Yes, children are welcome. We encourage nursing babies to join mothers at the meetings.
Can I bring my mother/mother-in-law/husband/other support person?
In general, we welcome support people to come. It is preferred that male support people do not attend the bulk of the meeting but instead come in at the very beginning of a meeting or at the very end.
Do you make home visits?
Some Leaders do make home visits, but it is not required of LLL Leaders. If you need help immediately, and the next LLL meeting in your area is not soon enough, contact a Leader in your area to see if there are any nearby Leaders who will meet with you.
Breastfeeding Questions
(excerpts edited for this site from Breastfeeding Tips & Guide pamphlet by La Leche League International)
I'm pregnant. What do I need to know about breastfeeding?
Congratulations! It’s great that you’re thinking about breastfeeding, because it’s not only the biologically normal way to feed your baby, but a big help as you learn to mother your baby. There is almost nothing you can do that will affect your child’s whole life, emotionally and physically, as much as breastfeeding will.
Here are a few of the top reasons that breastfeeding is important for both you and your baby:
• Breastfeeding for even a few days reduces postpartum problems and gives your baby’s kidneys, intestines, and liver a much healthier start. Your early milk is chock-full of protection that your baby will rely on for months to come. It has specially-tailored immunities that no formula can offer.
• If you breastfeed for more than a few months, you’ll be less likely than formula feeding mothers to develop certain cancers, diabetes, osteoporosis, and urinary tract infections.
• A diet of your milk alone for about the first six months of life helps ensure that your baby has a normal immune system, and protects him against many diseases and illnesses that are more likely with formula-feeding. That means a happier baby and fewer sick days away from your job.
• Breastfed babies use nursing for comfort and security as much as for food, so they tend to cry less.
• The longer you nurse, the better for your baby’s IQ and health, including long-term health risks such as cancers, heart disease, diabetes, and obesity.
• If you breastfeed exclusively, your fertility and menstrual periods usually don’t return for six months or more.
• You may be more likely to lose weight gradually without dieting while breastfeeding.
• Formula-feeding takes more time, effort, and money compared to breastfeeding.
• Breastfed babies tend to have silky, soft skin. Formula-fed babies are more likely to have eczema. They have more asthma and allergies, too.
• Breastfed babies’ stools smell much better.
• Lots of mothers wish they had breastfed. Very few breastfeeding mothers wish they had formula-fed. You can learn much more about every aspect of breastfeeding in La Leche League International’s book, The Womanly Art of Breastfeeding, 8th edition. It’s a great resource and a fun read.
Congratulations! It’s great that you’re thinking about breastfeeding, because it’s not only the biologically normal way to feed your baby, but a big help as you learn to mother your baby. There is almost nothing you can do that will affect your child’s whole life, emotionally and physically, as much as breastfeeding will.
Here are a few of the top reasons that breastfeeding is important for both you and your baby:
• Breastfeeding for even a few days reduces postpartum problems and gives your baby’s kidneys, intestines, and liver a much healthier start. Your early milk is chock-full of protection that your baby will rely on for months to come. It has specially-tailored immunities that no formula can offer.
• If you breastfeed for more than a few months, you’ll be less likely than formula feeding mothers to develop certain cancers, diabetes, osteoporosis, and urinary tract infections.
• A diet of your milk alone for about the first six months of life helps ensure that your baby has a normal immune system, and protects him against many diseases and illnesses that are more likely with formula-feeding. That means a happier baby and fewer sick days away from your job.
• Breastfed babies use nursing for comfort and security as much as for food, so they tend to cry less.
• The longer you nurse, the better for your baby’s IQ and health, including long-term health risks such as cancers, heart disease, diabetes, and obesity.
• If you breastfeed exclusively, your fertility and menstrual periods usually don’t return for six months or more.
• You may be more likely to lose weight gradually without dieting while breastfeeding.
• Formula-feeding takes more time, effort, and money compared to breastfeeding.
• Breastfed babies tend to have silky, soft skin. Formula-fed babies are more likely to have eczema. They have more asthma and allergies, too.
• Breastfed babies’ stools smell much better.
• Lots of mothers wish they had breastfed. Very few breastfeeding mothers wish they had formula-fed. You can learn much more about every aspect of breastfeeding in La Leche League International’s book, The Womanly Art of Breastfeeding, 8th edition. It’s a great resource and a fun read.
How often will my baby nurse?
Most newborns are ready to nurse in the first hour after birth. Nursing tends to go better if they get a chance to latch onto at least one breast during this time. After the first nursing, you’ll both probably feel sleepy for a while, so the next feeding may not happen for four to six hours. This is fine for full-term newborns. Some will nurse more often, and that’s fine, too. After the first twenty-four hours, a full-term, healthy newborn may need to nurse as often as several times an hour or as infrequently as every three hours, counting from the start of the feeding until the start of the next one. Expect to nurse your baby at least eight to twelve times every 24 hours.
Frequent feedings are important for the following reasons:
• They provide the nutrition your baby needs. Your milk was designed to be digested quickly and easily. These frequent, small amounts of colostrum, your first milk, are perfect for your baby’s tiny stomach.
• Frequent feedings ensure that your breasts are stimulated enough to establish a full milk supply. The more milk that is removed from your breasts, the more milk your body will produce.
• The security of your arms and breasts help your baby as he learns to live outside your body.
And don’t worry, feedings won’t always be this frequent. Your baby is not yet very efficient at nursing, and he’s growing rapidly. He’ll eat less often as he grows.
Many babies “cluster nurse,” which means they nurse often for a few hours and then sleep for several hours. Some babies also sleep for one long four to five hour stretch each day (ideally at night!). The number of feedings in a 24-hour period is more important than the spacing of feedings. You can’t nurse your baby “too often,” but you can nurse him too little. The best advice is to watch your baby, not your clock.
Signs of hunger include:
• bringing hands to mouth
• turning his head to the side, with wide, searching mouth
• chewing or sucking on hands or fingers
• bobbing head and mouth against your shoulder
• “Uh, uh, uh” sounds
Don’t wait for your baby to cry to let you know he is hungry. Crying is a very late hunger sign, and can make it harder for your baby to nurse effectively.
A sleepy baby may need to be wakened every two to three hours to feed at first, especially if he has jaundice or hasn’t been getting enough milk. Talk with your health care provider if your baby is difficult to wake for feedings.
Some babies seem to nurse all the time because they aren’t getting milk efficiently. If you feel your baby spends too much time nursing, be sure to check with your La Leche League Leader or an International Board Certified Lactation Consultant (IBCLC).
Waiting for your breast to feel full before your baby nurses can decrease your milk supply because you make milk more slowly when your breast is full. When you nurse frequently so that your breasts are softer, you’re actually making milk faster.
How do we get started?
In the early days, you and your baby are learning a new skill. It’s like riding a bicycle. You wobble, start over, wobble… but with practice it soon becomes second nature. So expect that it might take some time for both of you to figure it out.
To get started, make sure your baby is calm. Walk around with him if you need to, talk to him, stroke him, soothe him. Then find a position that you can be comfortable in for the whole feeding, and that allows both you and your baby to tap into your natural nursing instincts and reflexes.
In the early days, you and your baby are learning a new skill. It’s like riding a bicycle. You wobble, start over, wobble… but with practice it soon becomes second nature. So expect that it might take some time for both of you to figure it out.
To get started, make sure your baby is calm. Walk around with him if you need to, talk to him, stroke him, soothe him. Then find a position that you can be comfortable in for the whole feeding, and that allows both you and your baby to tap into your natural nursing instincts and reflexes.
|
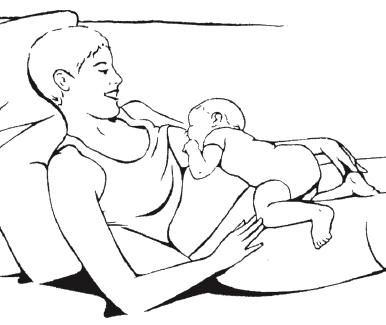
Using Gravity
• Try leaning back or semi-reclining on a bed, chair, or sofa, the way you would slouch to watch television. Not flat, but not fully upright. If you’re on a sofa, you can either stretch out across it or sit with your bottom near the edge and your shoulders against the back. Use pillows as needed to feel completely comfortable and fully supported. • Position your baby so that he is lying flat on his tummy with his head a little higher than his bottom and his feet touching your thigh (you may have to bend your knee to bring it close enough) and his cheek or mouth near one of your nipples. • Think of the arm that’s closest to that breast as the “rail” that keeps your baby from rolling onto his side. You’ll probably find that this arm naturally holds his back or bottom. • Feel free to use your other hand to help him latch by lifting or moving your nipple toward his mouth, but trust him to feel his way. He may even bob his head up and down like a woodpecker as he searches. If he’s been having trouble nursing, he may fuss and cry for a minute or two. Talk to him encouragingly as he figures out what to do. If he sucks on his hand, don’t pull it away – his hands help him relax and organize himself for nursing. • When his chin or cheek has solid contact with your breast, he’ll probably open his mouth and draw your nipple in. • Babies can crawl forward but they have trouble backing up. If he pushes himself past your nipple, try repositioning him. • Babies do best if they have to tip their head back a little to nurse, rather than having to tuck their chin. |
While lying back like this is often helpful for newborns, it isn’t something mothers of older babies usually need. When nursing is going well, you’ll eventually get to the point where your baby latches easily in just about any position. But finding a comfortable position is always important, and gravity can be your friend in achieving it – so often you will find yourself leaning back, resting your arms on your thighs, or using pillows to help you recline.
If lying back isn’t working for you, try one of these more mother-guided approaches. You may find that once your baby latches, you can lean back into a more comfortable position for the rest of the feeding.
If lying back isn’t working for you, try one of these more mother-guided approaches. You may find that once your baby latches, you can lean back into a more comfortable position for the rest of the feeding.
What should I do if my newborn can’t latch?
It can be frustrating and upsetting when a baby doesn’t latch easily. Here are some ideas that might help:
• First try the “gravity” position described above and see what your baby can do when he takes the lead (but don’t hesitate to move your breast to help him find the nipple).
• Try nursing when your baby is asleep or very sleepy.
• Change positions. Some babies prefer certain positions, at least at first.
• Try standing up and walking or swaying a little bit while bringing him toward the breast.
• Nurse in a quiet room with no distractions.
• Nurse in a noisy room with lots of distractions.
• Try spending time skin-to-skin – with your baby wearing just a diaper and snuggled against your bare chest. Use a blanket around both of you if the room is chilly.
• Sleep next to your baby (Reduce sleeping hazards - for more information on evaluating the safest sleep for your baby see Sweet Sleep from LLLI)
Check The Womanly Art of Breastfeeding, 8th edition, for more ideas, or contact an LLL Leader or International Board Certified Lactation Consultant (IBCLC) right away for help if your baby is still not latching well, to make sure that your baby is getting enough milk.
It can be frustrating and upsetting when a baby doesn’t latch easily. Here are some ideas that might help:
• First try the “gravity” position described above and see what your baby can do when he takes the lead (but don’t hesitate to move your breast to help him find the nipple).
• Try nursing when your baby is asleep or very sleepy.
• Change positions. Some babies prefer certain positions, at least at first.
• Try standing up and walking or swaying a little bit while bringing him toward the breast.
• Nurse in a quiet room with no distractions.
• Nurse in a noisy room with lots of distractions.
• Try spending time skin-to-skin – with your baby wearing just a diaper and snuggled against your bare chest. Use a blanket around both of you if the room is chilly.
• Sleep next to your baby (Reduce sleeping hazards - for more information on evaluating the safest sleep for your baby see Sweet Sleep from LLLI)
Check The Womanly Art of Breastfeeding, 8th edition, for more ideas, or contact an LLL Leader or International Board Certified Lactation Consultant (IBCLC) right away for help if your baby is still not latching well, to make sure that your baby is getting enough milk.
How long should nursing sessions last?
It’s hard to say how long a feeding should be because each mother’s breasts and each baby are different. Some mothers release their milk more easily and some babies nurse more effectively. Mothers have different amounts of milk at different times during the day. This means that no one can ever say how long a feeding should last and feedings should never be restricted to a certain number of minutes on each side. For babies who nurse eight to twelve times in 24 hours, most feedings last thirty to forty minutes in the first few weeks and months until babies become more experienced and efficient. Babies who nurse more often usually nurse for shorter times.
If you find that nursings take longer than this or your baby falls asleep after only few sucks, talk to a La Leche League Leader who can help you determine if there is a problem that needs further investigation.
It’s hard to say how long a feeding should be because each mother’s breasts and each baby are different. Some mothers release their milk more easily and some babies nurse more effectively. Mothers have different amounts of milk at different times during the day. This means that no one can ever say how long a feeding should last and feedings should never be restricted to a certain number of minutes on each side. For babies who nurse eight to twelve times in 24 hours, most feedings last thirty to forty minutes in the first few weeks and months until babies become more experienced and efficient. Babies who nurse more often usually nurse for shorter times.
If you find that nursings take longer than this or your baby falls asleep after only few sucks, talk to a La Leche League Leader who can help you determine if there is a problem that needs further investigation.
Which breast should I start on?
There are no rules about this. Using the fuller breast gives your baby more milk right away. Sometimes the softer breast gives your baby slower-flowing milk when he wants comfort nursing. Sometimes both breasts feel the same. You’ll learn when it matters and when it doesn’t. And you can always switch!
There are no rules about this. Using the fuller breast gives your baby more milk right away. Sometimes the softer breast gives your baby slower-flowing milk when he wants comfort nursing. Sometimes both breasts feel the same. You’ll learn when it matters and when it doesn’t. And you can always switch!
When should I switch sides?
There are no rules about this, either. If your baby starts to fuss, you might want to switch him to the other side. Or you can firmly (but not uncomfortably) squeeze your breast between your fingers and thumb to move the milk more quickly. Your baby may or may not want the other side. You can also switch sides just because you want to. Remember, there are no rules. But there are a lot more breastfeeding tips that mothers have learned over the years. We’ve collected many of them in The Womanly Art of Breastfeeding, 8th edition.
There are no rules about this, either. If your baby starts to fuss, you might want to switch him to the other side. Or you can firmly (but not uncomfortably) squeeze your breast between your fingers and thumb to move the milk more quickly. Your baby may or may not want the other side. You can also switch sides just because you want to. Remember, there are no rules. But there are a lot more breastfeeding tips that mothers have learned over the years. We’ve collected many of them in The Womanly Art of Breastfeeding, 8th edition.
What should I do if my nipples hurt?
Breastfeeding should never be more than mildly tender. If your nipples hurt, first try lying back more, as described in “How do we get started?” (above) and let your baby lead the way. When a baby nurses in this position, he’s on top of your breast. Gravity helps his jaw drop open wide so he can get a deeper latch – and that often means less pain. If this doesn’t help, or if your nipples have blisters or open wounds, contact an LLL Leader or International Board Certified Lactation Consultant (IBCLC) for help with positioning or to take a closer look at your baby’s mouth. Sometimes the problem is how your baby’s tongue moves, not how you’re nursing.
While you’re working to solve the problem, here are some ideas that can help with healing.
• Gently rub a few drops of your milk on your nipples after nursing and let them air dry. You can also use a tiny amount of over-the-counter antibiotic ointment after nursing. No need to wash it off before nursing again.
• Or use hydrogel pads tucked in your bra or under a snug-fitting tank top between nursings to relieve pain and promote healing. Hydrogel pads for nursing mothers are available at most baby and drug stores.
• Wash any nipple wounds with soap and water two or three times a day, to reduce the possibility of infection.
If you feel like you can’t continue nursing on painful nipples, contact a Leader or International Board Certified Lactation Consultant (IBCLC) right away for strategies to maintain your milk supply and address the underlying problem.
Breastfeeding should never be more than mildly tender. If your nipples hurt, first try lying back more, as described in “How do we get started?” (above) and let your baby lead the way. When a baby nurses in this position, he’s on top of your breast. Gravity helps his jaw drop open wide so he can get a deeper latch – and that often means less pain. If this doesn’t help, or if your nipples have blisters or open wounds, contact an LLL Leader or International Board Certified Lactation Consultant (IBCLC) for help with positioning or to take a closer look at your baby’s mouth. Sometimes the problem is how your baby’s tongue moves, not how you’re nursing.
While you’re working to solve the problem, here are some ideas that can help with healing.
• Gently rub a few drops of your milk on your nipples after nursing and let them air dry. You can also use a tiny amount of over-the-counter antibiotic ointment after nursing. No need to wash it off before nursing again.
• Or use hydrogel pads tucked in your bra or under a snug-fitting tank top between nursings to relieve pain and promote healing. Hydrogel pads for nursing mothers are available at most baby and drug stores.
• Wash any nipple wounds with soap and water two or three times a day, to reduce the possibility of infection.
If you feel like you can’t continue nursing on painful nipples, contact a Leader or International Board Certified Lactation Consultant (IBCLC) right away for strategies to maintain your milk supply and address the underlying problem.
What’s a normal nursing like?
When a baby first latches, he may do some quick sucks, pause, do more quick sucks, and pause again. Within a half minute or so, a baby who’s nursing well will begin to have longer, slower sucks with swallows following every one to three sucks as your milk releases (lets down). With each swallow, you’ll probably hear a whispered “keh” sound. Babies naturally pause after every dozen or so swallows, just as you pause during your own meals.
If you see very few long sucks or don’t hear many swallows, or if your nipples hurt, check with your breastfeeding helper for ideas. Otherwise, if it’s comfortable for both of you, you see or hear him swallowing, he ends the feeding looking relaxed and “milk drunk,” and your breasts feel lighter, you can be reassured that the feeding went well.
When a baby first latches, he may do some quick sucks, pause, do more quick sucks, and pause again. Within a half minute or so, a baby who’s nursing well will begin to have longer, slower sucks with swallows following every one to three sucks as your milk releases (lets down). With each swallow, you’ll probably hear a whispered “keh” sound. Babies naturally pause after every dozen or so swallows, just as you pause during your own meals.
If you see very few long sucks or don’t hear many swallows, or if your nipples hurt, check with your breastfeeding helper for ideas. Otherwise, if it’s comfortable for both of you, you see or hear him swallowing, he ends the feeding looking relaxed and “milk drunk,” and your breasts feel lighter, you can be reassured that the feeding went well.
Is my breastfed baby getting enough milk?
You can tell that your baby is getting enough by keeping track of stools, weight gain, and overall appearance. Most breastfed babies will have at least three bowel movements every 24 hours for the first month. Older babies may switch to less frequent but large bowel movements.
An average-sized baby will usually gain about an ounce a day after the fourth day of life, or about a half pound per week.
If your baby is not gaining well, or if he is losing weight after the first few days, first contact your baby’s doctor and then try some of these tips to increase the amount of milk your baby gets.
• Nurse often for as long as baby will nurse. If nursings take more than 30 to 45 minutes, have a breastfeeding helper check how well your baby is feeding.
• Firmly (but comfortably) squeeze your breast between your fingers and thumb to move the milk more quickly as your baby nurses.
• Have a breastfeeding session assessed by an experienced LLL Leader or International Board Certified Lactation Consultant (IBCLC).
You can tell that your baby is getting enough by keeping track of stools, weight gain, and overall appearance. Most breastfed babies will have at least three bowel movements every 24 hours for the first month. Older babies may switch to less frequent but large bowel movements.
An average-sized baby will usually gain about an ounce a day after the fourth day of life, or about a half pound per week.
If your baby is not gaining well, or if he is losing weight after the first few days, first contact your baby’s doctor and then try some of these tips to increase the amount of milk your baby gets.
• Nurse often for as long as baby will nurse. If nursings take more than 30 to 45 minutes, have a breastfeeding helper check how well your baby is feeding.
• Firmly (but comfortably) squeeze your breast between your fingers and thumb to move the milk more quickly as your baby nurses.
• Have a breastfeeding session assessed by an experienced LLL Leader or International Board Certified Lactation Consultant (IBCLC).
Why are my breasts uncomfortable four days after my baby’s birth?
Before your baby is born, your body starts making colostrum, a thick, yellowish, clear type of milk that provides your baby with immunities and helps prevent jaundice. By about the third day, your milk “comes in,” increasing in volume and gradually becoming whiter. As your milk becomes plentiful, your breasts may seem very full. The extreme fullness (engorgement) should subside in 12 to 48 hours.
Here are some ideas for minimizing engorgement:
• Nurse early and often. This means nursing in the first hour after birth and then offering to nurse whenever your baby shows any hunger cues (see "How Often will my Baby Nurse?" above),
• If your newborn sleeps longer than two to three hours in the day or four hours at night, wake him to nurse. If talking, stroking, undressing him, changing his diaper, and gentle handling don’t rouse him, try laying him on a flat surface and rolling him slowly and gently from side to side. Or put him skin-to-skin on your chest. Dimming the room often helps, too.
• Use cold compresses (or a bag of frozen vegetables) on your breasts between nursings, or put washed cabbage leaves directly over your breasts inside a bra. Change them when they wilt.
• Before nursing, put a warm, moist cloth on your breast and express some milk to make latching easier.
• Use “Reverse Pressure Softening.” Place your fingertips in a ring at the base of your nipple and press down for thirty seconds or so to soften that part of your breast temporarily, then quickly offer your breast to your baby.
Contact your health care provider if:
• you still feel discomfort after trying the above tips.
• you have a fever of 101°F or more, red/painful/swollen breast(s), or “flu-like” symptoms.
• your baby is unable to latch to your breast.
• after day three or four, your baby is not having three or four stools each day. By the end of a week or so, expect five or six stools each day until your baby is about a month old (when stools may become larger but less frequent).
Before your baby is born, your body starts making colostrum, a thick, yellowish, clear type of milk that provides your baby with immunities and helps prevent jaundice. By about the third day, your milk “comes in,” increasing in volume and gradually becoming whiter. As your milk becomes plentiful, your breasts may seem very full. The extreme fullness (engorgement) should subside in 12 to 48 hours.
Here are some ideas for minimizing engorgement:
• Nurse early and often. This means nursing in the first hour after birth and then offering to nurse whenever your baby shows any hunger cues (see "How Often will my Baby Nurse?" above),
• If your newborn sleeps longer than two to three hours in the day or four hours at night, wake him to nurse. If talking, stroking, undressing him, changing his diaper, and gentle handling don’t rouse him, try laying him on a flat surface and rolling him slowly and gently from side to side. Or put him skin-to-skin on your chest. Dimming the room often helps, too.
• Use cold compresses (or a bag of frozen vegetables) on your breasts between nursings, or put washed cabbage leaves directly over your breasts inside a bra. Change them when they wilt.
• Before nursing, put a warm, moist cloth on your breast and express some milk to make latching easier.
• Use “Reverse Pressure Softening.” Place your fingertips in a ring at the base of your nipple and press down for thirty seconds or so to soften that part of your breast temporarily, then quickly offer your breast to your baby.
Contact your health care provider if:
• you still feel discomfort after trying the above tips.
• you have a fever of 101°F or more, red/painful/swollen breast(s), or “flu-like” symptoms.
• your baby is unable to latch to your breast.
• after day three or four, your baby is not having three or four stools each day. By the end of a week or so, expect five or six stools each day until your baby is about a month old (when stools may become larger but less frequent).
What if my baby fusses when he starts nursing?
If you have a forceful milk release (the surge of milk at the beginning of a feeding), your breasts may be delivering more milk than your baby can handle. Some symptoms:
• Fussiness or restlessness at the breast; arching away from the breast during milk release.
• Coughing, sputtering, and spitting up while nursing.
• Gassiness, with green, watery, or explosive stools.
Talk with an LLL Leader to help you determine if a forceful milk release or oversupply is the problem. As long as your baby is gaining well, you may be able to reduce your supply slightly or help your baby manage your supply better with these ideas:
• When your baby stops nursing on the first breast, burp him and offer the second breast. He probably will take less milk from that breast and you can start with it the next time.
• Use a side-lying nursing position, which allows excess milk to dribble out of your baby’s mouth and may make nursing easier for him.
• Use the lying-back position so that your baby has more control during the feeding.
• Try nursing your baby while he straddles your legs.
• Nurse more frequently, which means smaller meals that may make feedings easier for your baby to manage.
• If none of these ideas help, try nursing from just one breast several times, until it feels completely soft, hand expressing just enough milk from the other breast to be comfortable. Then nurse from the other side several times to soften it completely. Keep alternating this way, with two or more nursings on each side.
If you have a forceful milk release (the surge of milk at the beginning of a feeding), your breasts may be delivering more milk than your baby can handle. Some symptoms:
• Fussiness or restlessness at the breast; arching away from the breast during milk release.
• Coughing, sputtering, and spitting up while nursing.
• Gassiness, with green, watery, or explosive stools.
Talk with an LLL Leader to help you determine if a forceful milk release or oversupply is the problem. As long as your baby is gaining well, you may be able to reduce your supply slightly or help your baby manage your supply better with these ideas:
• When your baby stops nursing on the first breast, burp him and offer the second breast. He probably will take less milk from that breast and you can start with it the next time.
• Use a side-lying nursing position, which allows excess milk to dribble out of your baby’s mouth and may make nursing easier for him.
• Use the lying-back position so that your baby has more control during the feeding.
• Try nursing your baby while he straddles your legs.
• Nurse more frequently, which means smaller meals that may make feedings easier for your baby to manage.
• If none of these ideas help, try nursing from just one breast several times, until it feels completely soft, hand expressing just enough milk from the other breast to be comfortable. Then nurse from the other side several times to soften it completely. Keep alternating this way, with two or more nursings on each side.
What can my partner do to help?
Breastfeeding is what mothers do, but there are lots of important ways your partner can bond with your baby and participate in his care. Some ideas:
• Comfort your baby by holding, rocking, or walking.
• Give your baby a massage.
• Hold your baby skin-to-skin.
• Play with your baby. Show the baby pictures around the house, sing songs, make silly conversation.
• Enjoy relaxing sleepy-baby-on-chest times.
• Use a soft carrier to take the baby on walks, outside or around the house.
• Change diapers and give baths. At first, some babies will fuss during diaper changes and baths. But they soon become a fun, sociable time for both baby and parent.
• Make meals, shop for groceries, and bring you snacks and drinks while you nurse.
• Run interference with difficult family or friends.
• Support your efforts to breastfeed. Being supportive of breastfeeding is the most important thing a partner can do – it helps your own confidence in your mothering and helps ensure that your baby gets a normal, happy start in life.
Breastfeeding is what mothers do, but there are lots of important ways your partner can bond with your baby and participate in his care. Some ideas:
• Comfort your baby by holding, rocking, or walking.
• Give your baby a massage.
• Hold your baby skin-to-skin.
• Play with your baby. Show the baby pictures around the house, sing songs, make silly conversation.
• Enjoy relaxing sleepy-baby-on-chest times.
• Use a soft carrier to take the baby on walks, outside or around the house.
• Change diapers and give baths. At first, some babies will fuss during diaper changes and baths. But they soon become a fun, sociable time for both baby and parent.
• Make meals, shop for groceries, and bring you snacks and drinks while you nurse.
• Run interference with difficult family or friends.
• Support your efforts to breastfeed. Being supportive of breastfeeding is the most important thing a partner can do – it helps your own confidence in your mothering and helps ensure that your baby gets a normal, happy start in life.
When will my baby sleep through the night?
There’s no way to predict when a baby will sleep through the night and there’s no “right age” at which he should. The medical definition of “sleeping through the night” is only a five-hour stretch. Most young babies need to nurse several times during the night to gain well. Your milk is designed to be digested quickly and easily, which means frequent nursing. So how can you get the sleep you need? Try to rest when your baby naps, even if you just put your feet up. Resist the temptation to use baby’s naptime to catch up on chores. Napping together on the bed is a lovely way to get some extra sleep.
Some experts recommend that the baby sleep in the same room as the parents but on a separate surface. If you find that this makes breastfeeding harder, remember that the safest arrangement of all is:
• a non-smoking,
• sober,
• breastfeeding mother,
• sharing sleep with her baby on a safe surface.
As a breastfeeding mother, you’ll probably do a “cuddle curl” around your baby. This is a safe, protective position for you and your baby. If you nurse lying down, your baby will naturally roll onto his back when he’s finished. You may find you do the same.
Here are a few more safety tips:
• Do NOT sleep with your baby on a couch, recliner, or armchair. There are too many cracks and crevices he could slip into.
• Use a mattress firm enough that your baby doesn’t roll against you when you lie down.
• Remove potential hazards from your baby’s sleeping area (gaps he can get trapped in, blankets and pillows near the baby’s head, ties and strings on night clothes, stuffed toys, pets, and older children).
Avoid sharing a bed with your baby if:
• any person in the bed is a smoker. Exposure to cigarette smoke, even secondhand smoke, is a huge risk factor for Sudden Infant Death Syndrome (SIDS).
• any person in the bed has consumed alcohol or taken drugs (legal or illegal) that could make him/her extra sleepy.
• any person in the bed is too exhausted to be aware of the baby, or has a condition that affects his/her awareness of the baby.
Sleep and safety are so important. For more information about making safe sleep choices, check out the book Sweet Sleep from LLLI.
There’s no way to predict when a baby will sleep through the night and there’s no “right age” at which he should. The medical definition of “sleeping through the night” is only a five-hour stretch. Most young babies need to nurse several times during the night to gain well. Your milk is designed to be digested quickly and easily, which means frequent nursing. So how can you get the sleep you need? Try to rest when your baby naps, even if you just put your feet up. Resist the temptation to use baby’s naptime to catch up on chores. Napping together on the bed is a lovely way to get some extra sleep.
Some experts recommend that the baby sleep in the same room as the parents but on a separate surface. If you find that this makes breastfeeding harder, remember that the safest arrangement of all is:
• a non-smoking,
• sober,
• breastfeeding mother,
• sharing sleep with her baby on a safe surface.
As a breastfeeding mother, you’ll probably do a “cuddle curl” around your baby. This is a safe, protective position for you and your baby. If you nurse lying down, your baby will naturally roll onto his back when he’s finished. You may find you do the same.
Here are a few more safety tips:
• Do NOT sleep with your baby on a couch, recliner, or armchair. There are too many cracks and crevices he could slip into.
• Use a mattress firm enough that your baby doesn’t roll against you when you lie down.
• Remove potential hazards from your baby’s sleeping area (gaps he can get trapped in, blankets and pillows near the baby’s head, ties and strings on night clothes, stuffed toys, pets, and older children).
Avoid sharing a bed with your baby if:
• any person in the bed is a smoker. Exposure to cigarette smoke, even secondhand smoke, is a huge risk factor for Sudden Infant Death Syndrome (SIDS).
• any person in the bed has consumed alcohol or taken drugs (legal or illegal) that could make him/her extra sleepy.
• any person in the bed is too exhausted to be aware of the baby, or has a condition that affects his/her awareness of the baby.
Sleep and safety are so important. For more information about making safe sleep choices, check out the book Sweet Sleep from LLLI.
How do we start solid foods?
Around the middle of the first year, your baby will begin to show you that he’s ready to start solid foods. Some signs include:
• sitting without support.
• reaching for objects and bringing them to his mouth.
• getting finger foods to his mouth, chewing them, liking them, and reaching for more.
Babies eat the most safely when they feed themselves. If you’re not sure if your baby is ready, let him sit next to you at the table with appropriate food in front of him. When he’s mature enough to eat it, he’ll eat it! It’s as simple as that! You can help with a spoon here and there, but your baby will have the most fun and learn the fastest if he handles most of the solids on his own. And you’ll probably find that waiting until he can feed himself is less messy.
Your baby’s first meals won’t be very big – maybe only a bite or two, with plenty of smearing and experimenting. He’ll still need to nurse as his main source of nourishment for many more months. To make sure your baby continues to get enough milk while he transitions to solids, nurse him first, offer the solid food, then nurse again.
Good early foods include:
• pieces of banana, baked or steamed sweet potato “sticks,” and avocado diced into small pieces that are easy to pick up.
• other soft fruits like ripe plums, peaches, and pears. They may be easier for your baby to handle if the skin is left on. You’ll find he spits out what he can’t chew.
• cooked vegetables like green beans, broccoli, peas, and carrots.
• protein-rich foods like chicken, fish, or beans, cooked until tender.
• whole grain cereals, breads, and crackers
Foods that have a “handle” (like a broccoli floret or carrot stick) or that are large enough for the baby to hold two-handed (like a small pear) are easiest for your beginning eater to manage.
Around the middle of the first year, your baby will begin to show you that he’s ready to start solid foods. Some signs include:
• sitting without support.
• reaching for objects and bringing them to his mouth.
• getting finger foods to his mouth, chewing them, liking them, and reaching for more.
Babies eat the most safely when they feed themselves. If you’re not sure if your baby is ready, let him sit next to you at the table with appropriate food in front of him. When he’s mature enough to eat it, he’ll eat it! It’s as simple as that! You can help with a spoon here and there, but your baby will have the most fun and learn the fastest if he handles most of the solids on his own. And you’ll probably find that waiting until he can feed himself is less messy.
Your baby’s first meals won’t be very big – maybe only a bite or two, with plenty of smearing and experimenting. He’ll still need to nurse as his main source of nourishment for many more months. To make sure your baby continues to get enough milk while he transitions to solids, nurse him first, offer the solid food, then nurse again.
Good early foods include:
• pieces of banana, baked or steamed sweet potato “sticks,” and avocado diced into small pieces that are easy to pick up.
• other soft fruits like ripe plums, peaches, and pears. They may be easier for your baby to handle if the skin is left on. You’ll find he spits out what he can’t chew.
• cooked vegetables like green beans, broccoli, peas, and carrots.
• protein-rich foods like chicken, fish, or beans, cooked until tender.
• whole grain cereals, breads, and crackers
Foods that have a “handle” (like a broccoli floret or carrot stick) or that are large enough for the baby to hold two-handed (like a small pear) are easiest for your beginning eater to manage.
Is there anything I should or shouldn’t eat while breastfeeding?
A healthy diet keeps you feeling good, but your milk is always right for your baby no matter what you eat. In general, no food is off-limits for a breastfeeding mother. Just use common sense: if you notice that your baby reacts badly after something you’ve eaten, it may be best to leave that food out of your diet for a while. The amount of caffeine in five or fewer five-ounce cups of coffee doesn’t usually cause a problem for most moms and babies after the first month or so. You’ll know that you’ve had too much or your baby is especially sensitive because a baby who is being over-stimulated with caffeine will be wide-eyed, active, alert, and fussy.
A healthy diet keeps you feeling good, but your milk is always right for your baby no matter what you eat. In general, no food is off-limits for a breastfeeding mother. Just use common sense: if you notice that your baby reacts badly after something you’ve eaten, it may be best to leave that food out of your diet for a while. The amount of caffeine in five or fewer five-ounce cups of coffee doesn’t usually cause a problem for most moms and babies after the first month or so. You’ll know that you’ve had too much or your baby is especially sensitive because a baby who is being over-stimulated with caffeine will be wide-eyed, active, alert, and fussy.
What about alcohol?
Alcohol is not good for babies, but most mothers can drink in moderation while breastfeeding. Alcohol does transfer into the milk, but it also passes out of the milk so that there’s no need to “pump and dump.” It takes a 120-pound woman about three hours to eliminate the majority of the alcohol from her blood (and thus her milk) in each serving of beer or wine, so multiply the number of drinks you have by three to know how many hours it will take until your milk is mostly alcohol free again.
You can’t rush the process by “pumping and dumping” or drinking a lot of water or coffee. If you’ve had so much to drink that your baby needs to be fed before your milk is mostly alcohol-free, it’s better to used previously pumped (alcohol free) milk than formula. Even a little bit of formula reduces your baby’s immune system and may have other harmful effects.
Recreational drugs pass into the milk and can be dangerous to your baby. Depending on the drug, it may take quite a long time for it to pass out of the milk and your system. During this time, you may not be alert enough to care for your baby. For these reasons, it’s best not to use recreational drugs while you’re breastfeeding or caring for children.
Alcohol is not good for babies, but most mothers can drink in moderation while breastfeeding. Alcohol does transfer into the milk, but it also passes out of the milk so that there’s no need to “pump and dump.” It takes a 120-pound woman about three hours to eliminate the majority of the alcohol from her blood (and thus her milk) in each serving of beer or wine, so multiply the number of drinks you have by three to know how many hours it will take until your milk is mostly alcohol free again.
You can’t rush the process by “pumping and dumping” or drinking a lot of water or coffee. If you’ve had so much to drink that your baby needs to be fed before your milk is mostly alcohol-free, it’s better to used previously pumped (alcohol free) milk than formula. Even a little bit of formula reduces your baby’s immune system and may have other harmful effects.
Recreational drugs pass into the milk and can be dangerous to your baby. Depending on the drug, it may take quite a long time for it to pass out of the milk and your system. During this time, you may not be alert enough to care for your baby. For these reasons, it’s best not to use recreational drugs while you’re breastfeeding or caring for children.
Is it safe to breastfeed if I’m sick or taking medication?
Mothers can safely breastfeed their babies through a variety of illnesses, from colds and infections to chronic conditions. Your body makes antibodies to combat an illness and these antibodies are passed directly to baby through your milk, giving protection and disease-fighting abilities to your baby. Most medications are compatible with breastfeeding, but every situation is unique. If your doctor prescribes a medication or you want to take an over-the-counter drug, you can use LactMed to find specific information about the drug’s effect on breastfeeding. The Infant Risk Center also has a hotline Monday – Friday, 8am – 5pm CT (806) 352-2519.
Mothers can safely breastfeed their babies through a variety of illnesses, from colds and infections to chronic conditions. Your body makes antibodies to combat an illness and these antibodies are passed directly to baby through your milk, giving protection and disease-fighting abilities to your baby. Most medications are compatible with breastfeeding, but every situation is unique. If your doctor prescribes a medication or you want to take an over-the-counter drug, you can use LactMed to find specific information about the drug’s effect on breastfeeding. The Infant Risk Center also has a hotline Monday – Friday, 8am – 5pm CT (806) 352-2519.
How do I continue breastfeeding when I go back to work?
Leaving your baby to return to work can be tough, regardless of how you feed your baby. The more time you can take off after your baby is born, the more time you will have to get breastfeeding established. Breastfeeding exclusively while you are at home establishes your milk supply and helps both of you learn your own style. Here are some other tips that may help:
• Wait to introduce a bottle until you’re both nursing with confidence. Check with your La Leche League Leader for some gentle approaches.
• Discuss with your partner who will be responsible for shopping, cooking, changing diapers, and other jobs. What expectations does each of you have?
• Do as much as possible each night, such as preparing the diaper bag, laying out clothes, and talking over the next day’s game plan with your partner.
• Practice pumping or hand expressing your milk so you learn what works for you. Start by expressing after the first feeding in the morning when your supply is highest.
• Freeze the expressed milk to use for your first few days back at work (be sure to write the date you expressed it on the bag).
• You can start storing milk as soon as breastfeeding is going smoothly, but remember that you won’t need a freezer-full ahead of time. Each day’s pumping should provide enough milk for the next day’s time at daycare.
• Talk with other mothers about their experiences with returning to work while breastfeeding. To find a La Leche League group in Nebraska head back to our main page.
• Make the first week back at work a short one by returning late in the week.
• If you can, take the next Wednesday off. You’ll work no more than two days in a row for a week and a half!
• Plan to express your milk at least twice – maybe three times – while you’re at work.
• Talk with your employer about your needs and schedule. This will give you a chance to develop a workable plan for both of you. Mention that breastfeeding mothers take less time off from their jobs to care for a sick baby because their babies are healthier!
• Some mothers arrange to see their baby during lunch or at a break, so they can nurse instead of expressing milk during that part of the work day.
• Two-piece outfits make pumping or hand expression easier while at work.
• Wearing a jacket or sweater will hide evidence of leaking. Breast pads may help, particularly in the first weeks back at work.
Leaving your baby to return to work can be tough, regardless of how you feed your baby. The more time you can take off after your baby is born, the more time you will have to get breastfeeding established. Breastfeeding exclusively while you are at home establishes your milk supply and helps both of you learn your own style. Here are some other tips that may help:
• Wait to introduce a bottle until you’re both nursing with confidence. Check with your La Leche League Leader for some gentle approaches.
• Discuss with your partner who will be responsible for shopping, cooking, changing diapers, and other jobs. What expectations does each of you have?
• Do as much as possible each night, such as preparing the diaper bag, laying out clothes, and talking over the next day’s game plan with your partner.
• Practice pumping or hand expressing your milk so you learn what works for you. Start by expressing after the first feeding in the morning when your supply is highest.
• Freeze the expressed milk to use for your first few days back at work (be sure to write the date you expressed it on the bag).
• You can start storing milk as soon as breastfeeding is going smoothly, but remember that you won’t need a freezer-full ahead of time. Each day’s pumping should provide enough milk for the next day’s time at daycare.
• Talk with other mothers about their experiences with returning to work while breastfeeding. To find a La Leche League group in Nebraska head back to our main page.
• Make the first week back at work a short one by returning late in the week.
• If you can, take the next Wednesday off. You’ll work no more than two days in a row for a week and a half!
• Plan to express your milk at least twice – maybe three times – while you’re at work.
• Talk with your employer about your needs and schedule. This will give you a chance to develop a workable plan for both of you. Mention that breastfeeding mothers take less time off from their jobs to care for a sick baby because their babies are healthier!
• Some mothers arrange to see their baby during lunch or at a break, so they can nurse instead of expressing milk during that part of the work day.
• Two-piece outfits make pumping or hand expression easier while at work.
• Wearing a jacket or sweater will hide evidence of leaking. Breast pads may help, particularly in the first weeks back at work.
How often should I express my milk if I’m away from my baby?
Start by expressing your milk about every three hours while you’re away, or about three times in an eight-hour day. You may find that two times is enough; most mothers need to express more than once. Expressing both breasts at the same time generally takes about 10 to 15 minutes. As your baby gets older and begins eating solids, you may not need to pump as frequently. If your baby is cared for nearby, you may be able to nurse instead of expressing milk. Your baby may sleep more while you’re apart, and nurse more when you’re together, including throughout the night (this is called “reverse cycling”). If this happens, eventually you may be able to pump or hand express milk less often when you are away.
Start by expressing your milk about every three hours while you’re away, or about three times in an eight-hour day. You may find that two times is enough; most mothers need to express more than once. Expressing both breasts at the same time generally takes about 10 to 15 minutes. As your baby gets older and begins eating solids, you may not need to pump as frequently. If your baby is cared for nearby, you may be able to nurse instead of expressing milk. Your baby may sleep more while you’re apart, and nurse more when you’re together, including throughout the night (this is called “reverse cycling”). If this happens, eventually you may be able to pump or hand express milk less often when you are away.
At work, you can just rinse your pump parts and bottles, but be sure to clean them thoroughly at the end of each day. Hot, soapy water or the dishwasher is fine. No need to sterilize for a breastfed baby. (Remember that great immune system!)
Can I hold my baby too much?
No! In the early months, babies need to be held close to their mothers as much as possible to feel secure and learn to trust. Babies who are not held much tend to cry more than babies who are carried next to their mothers’ bodies in baby carriers or wraps or in their arms. Holding a baby isn’t spoiling; it’s normal! The concept of “babywearing” – using slings, wraps, and soft carriers to keep the baby close while freeing your hands to do other tasks – has been popular in cultures around the world and throughout history because it keeps the baby happy while you get things done. Babywearing also can make it easier to nurse discreetly in public.
No! In the early months, babies need to be held close to their mothers as much as possible to feel secure and learn to trust. Babies who are not held much tend to cry more than babies who are carried next to their mothers’ bodies in baby carriers or wraps or in their arms. Holding a baby isn’t spoiling; it’s normal! The concept of “babywearing” – using slings, wraps, and soft carriers to keep the baby close while freeing your hands to do other tasks – has been popular in cultures around the world and throughout history because it keeps the baby happy while you get things done. Babywearing also can make it easier to nurse discreetly in public.
When I breastfeed in public...
Breastfeeding mothers have always nursed wherever they need to be. You don’t have to be stuck at home. It’s good for both you and your baby to get outside and enjoy the world, go about your normal errands, and meet up with friends. The beauty of breastfeeding is that you can do it all without having to think about bringing bottles and formula. All you need is an easy way to give your baby access to your breast without having to go through too many layers of clothes. Two piece outfits and tops that unbutton from the bottom work great. There are also outfits designed especially for breastfeeding conveniently in public. La Leche League International has partnered with Q-T Intimates to create a unique and affordable line of bras and apparel so moms can breastfeed with ease and comfort. See the line of apparel at lllibras.com.
If you’re concerned about nursing in public, here are some ideas to learn how to do it so that no one can tell (except another nursing mother):
• Practice “public” breastfeeding at home. Your partner, a close friend, or a mirror can give helpful feedback.
• Start slow – nurse at friends’ homes, then slightly more public places, then even more public places until you feel comfortable anywhere.
• Go to a La Leche League meeting. It’s the perfect place to connect with other mothers and see how they nurse in public.
Breastfeeding your baby is a basic right for both of you. Most states in the USA have laws that protect a mother’s right to breastfeed her baby in public. Check breastfeedinglaw.com for up-to-date information about legislation in your area.
Breastfeeding mothers have always nursed wherever they need to be. You don’t have to be stuck at home. It’s good for both you and your baby to get outside and enjoy the world, go about your normal errands, and meet up with friends. The beauty of breastfeeding is that you can do it all without having to think about bringing bottles and formula. All you need is an easy way to give your baby access to your breast without having to go through too many layers of clothes. Two piece outfits and tops that unbutton from the bottom work great. There are also outfits designed especially for breastfeeding conveniently in public. La Leche League International has partnered with Q-T Intimates to create a unique and affordable line of bras and apparel so moms can breastfeed with ease and comfort. See the line of apparel at lllibras.com.
If you’re concerned about nursing in public, here are some ideas to learn how to do it so that no one can tell (except another nursing mother):
• Practice “public” breastfeeding at home. Your partner, a close friend, or a mirror can give helpful feedback.
• Start slow – nurse at friends’ homes, then slightly more public places, then even more public places until you feel comfortable anywhere.
• Go to a La Leche League meeting. It’s the perfect place to connect with other mothers and see how they nurse in public.
Breastfeeding your baby is a basic right for both of you. Most states in the USA have laws that protect a mother’s right to breastfeed her baby in public. Check breastfeedinglaw.com for up-to-date information about legislation in your area.
If I stopped breastfeeding, can I start again?
Yes! Lots of women have done exactly that. But you’ll be much more likely to succeed if you work with a La Leche League Leader or IBCLC, who can help you increase your milk supply and keep your baby well-fed.
Yes! Lots of women have done exactly that. But you’ll be much more likely to succeed if you work with a La Leche League Leader or IBCLC, who can help you increase your milk supply and keep your baby well-fed.
How does my baby wean?
Mothers and babies can nurse as long as they want to, even if it’s a different length from what their friends or relatives do. Every drop of milk and every nursing time matters to your baby, and there’s no upper limit to how long a baby “should” nurse. Health agencies around the world agree that breastfeeding should continue for at least the first year, and for as long after that as mother and child desire. The World Health Organization recommends breastfeeding for two years and for longer if possible. Your own experience is almost certainly going to be different from what you planned.
Weaning abruptly is almost never necessary; it’s worth a second opinion from someone who understands both your situation and breastfeeding. If you do have to wean suddenly, it’s best to reduce your milk supply as slowly as you can to avoid a breast infection. When your breasts begin to feel uncomfortably full, remove just enough milk to feel comfortable again. This will help you stay comfortable while giving your breasts the signal to shut down production. It may take a week to ten days to feel like you don’t have to remove any more milk.
If you need to wean before a year, you’ll probably replace your breasts with bottles. Drop one nursing every few days and substitute a bottle to help your breasts and your baby adjust gradually.
Weaning a baby older than a year means you can probably skip formula altogether, though you’ll still need alternative ways to comfort, reassure, and connect. A time honored way to encourage weaning is “don’t offer, don’t refuse.” You stop offering the breast voluntarily, but you don’t refuse if he asks for it. It helps to avoid the places where you usually sit down to nurse, spots that mean “nursing time.”
Weaning naturally occurs very gradually as you and your baby move into the next phase of your relationship. It happens automatically without any help from you. If your baby seems to be weaning abruptly or earlier than you expected, talk to your LLL Leader about what might be causing it.
Mothers and babies can nurse as long as they want to, even if it’s a different length from what their friends or relatives do. Every drop of milk and every nursing time matters to your baby, and there’s no upper limit to how long a baby “should” nurse. Health agencies around the world agree that breastfeeding should continue for at least the first year, and for as long after that as mother and child desire. The World Health Organization recommends breastfeeding for two years and for longer if possible. Your own experience is almost certainly going to be different from what you planned.
Weaning abruptly is almost never necessary; it’s worth a second opinion from someone who understands both your situation and breastfeeding. If you do have to wean suddenly, it’s best to reduce your milk supply as slowly as you can to avoid a breast infection. When your breasts begin to feel uncomfortably full, remove just enough milk to feel comfortable again. This will help you stay comfortable while giving your breasts the signal to shut down production. It may take a week to ten days to feel like you don’t have to remove any more milk.
If you need to wean before a year, you’ll probably replace your breasts with bottles. Drop one nursing every few days and substitute a bottle to help your breasts and your baby adjust gradually.
Weaning a baby older than a year means you can probably skip formula altogether, though you’ll still need alternative ways to comfort, reassure, and connect. A time honored way to encourage weaning is “don’t offer, don’t refuse.” You stop offering the breast voluntarily, but you don’t refuse if he asks for it. It helps to avoid the places where you usually sit down to nurse, spots that mean “nursing time.”
Weaning naturally occurs very gradually as you and your baby move into the next phase of your relationship. It happens automatically without any help from you. If your baby seems to be weaning abruptly or earlier than you expected, talk to your LLL Leader about what might be causing it.
Where can I find a support network to help me breastfeed?
In addition to your partner, family, and friends, you can find support and information through:
• The Womanly Art of Breastfeeding, 8th edition.
• a local La Leche League (LLL) Leader, an accredited volunteer who is there to help in person, over the phone, or online. A LLL Leader is always a good starting point for getting help and finding other resources.
• La Leche League International
• La Leche League International’s online community
• LLLI Breastfeeding Support Facebook Page
• La Leche League International on Facebook
• La Leche League cafés and meetings. Going while you’re pregnant gives you practical tips. Once your baby is born, being with other mothers is a big help in getting comfortable with breastfeeding and mothering. A La Leche Leader is always there, too, to answer your questions and concerns.
• An International Board Certified Lactation Consultant (IBCLC), who can work with you one-on-one with questions beyond the basics.
In addition to your partner, family, and friends, you can find support and information through:
• The Womanly Art of Breastfeeding, 8th edition.
• a local La Leche League (LLL) Leader, an accredited volunteer who is there to help in person, over the phone, or online. A LLL Leader is always a good starting point for getting help and finding other resources.
• La Leche League International
• La Leche League International’s online community
• LLLI Breastfeeding Support Facebook Page
• La Leche League International on Facebook
• La Leche League cafés and meetings. Going while you’re pregnant gives you practical tips. Once your baby is born, being with other mothers is a big help in getting comfortable with breastfeeding and mothering. A La Leche Leader is always there, too, to answer your questions and concerns.
• An International Board Certified Lactation Consultant (IBCLC), who can work with you one-on-one with questions beyond the basics.